A report issued by Demos "I LOVE THE NHS, BUT...": Preventing needless harms caused by poor communications in the NHS dissects a prevalent issue in the healthcare system—the critical lack of communication within the National Health Service (NHS). Initially cautious about disclosing their experiences, participants—encompassing patients, NHS staff, and the public—underwent a notable transformation when prompted to share their opinions about the NHS. With a focus on delivering feasible solutions, the report sheds light on how bolstering communication can support the NHS in effecting positive changes. Highlighting critical issues impacting both patients and staff, the report dismisses the notion that communication is a mere 'nice to have,' underscoring its fundamental role in the seamless functioning of the NHS. Continue reading below to discover the roadmap for change.
The communication issues surfaced through deliberative work with the British public, aimed at understanding their health and care priorities and developing those priorities into policies. The report delineates the experience of poor communication by patients and staff, illuminates its manifestation as a public priority, and discerns potential areas within the political landscape where action could be taken.
Identifying the Problem
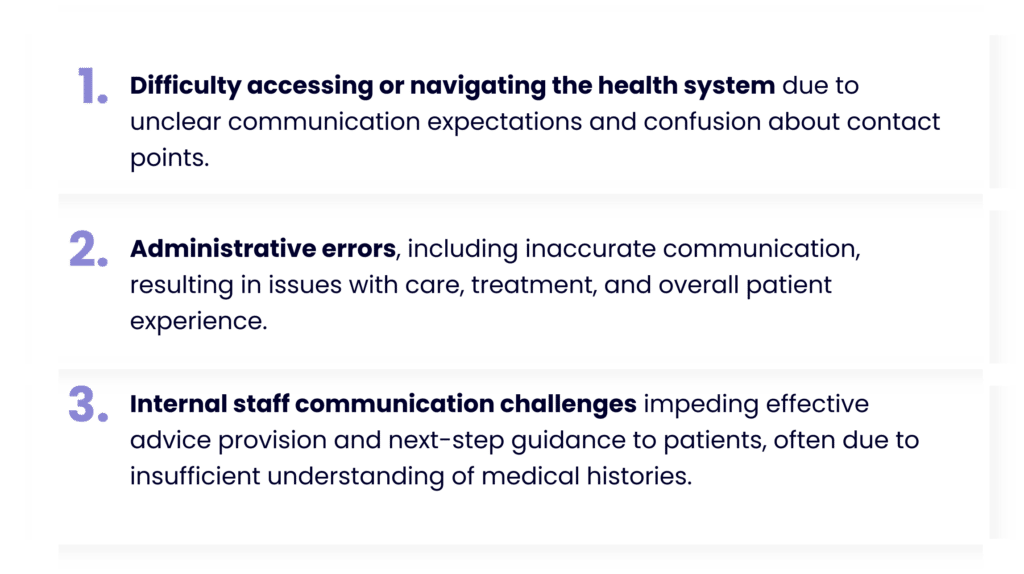
According to the report, these issues contribute to patient dissatisfaction, safety concerns, and mental health impacts. Surprisingly, despite being a significant concern for the public, poor communication ranks low on the political agenda.
“NHS, politicians and governments need a serious plan for how NHS communication will improve to improve patient experience and public confidence in the NHS. Public confidence in the NHS has deteriorated rapidly recently.”
Based on September 2023 polling, the report reveals that *over half (55%) of the UK public encountered poor communication issues within the NHS in the last five years. Patient survey results reveal disparities between expectations and experiences:
- 66% consider communication important in their care, but 41% are dissatisfied with communication from clinicians and staff.
- 68% find being listened to, believed, or taken seriously important, but only 38% feel treated this way.
- 61% emphasize the importance of coordination between different parts of the care system, but only 46% feel they experience it.
Report Findings
55%
of patients experienced poor communication in the last five years ¹
41%
of patients expressed dissatisfaction from clinicians and staff ²
30%
of patients stated that poor communication has damaged their trust in the NHS ³
¹ ³ “Developing a Data Pact: the relationship between the public, their data and the health and care system”, The Patients Association, September 2023, www.patients-association.org.uk/Handlers/Download.ashx?IDMF=c348045e-4ffc-43e5-a2ce-8a21ca1c6c5e
² “Being a Patient”, The Patients Association, July 2020, www.patients-association.org.uk/blog/new-report-being-a-patient
The results of poor communication between both patients and staff and between staff members themselves range from inconvenience and irritation, to significant negative outcomes for people’s health. Poor communication hinders patients' access to necessary care, contributes to treatment errors, and forces individuals to repeatedly explain their conditions. This breakdown in communication results in reduced satisfaction with the care provided.
According to the report, “The way the NHS is currently undertaking administration and bureaucracy is clearly failing to meet the needs of patients. This is a key driver of poor communication and a large part of the reason people need additional support to navigate the system”.While recent government initiatives indicate a growing awareness of the need for transformation, participants emphasize that the current administrative framework fails to meet patient needs, contributing to communication breakdowns and impeding meaningful patient involvement in care decisions. The report underscores the imperative for policymakers to confront the scale of the administrative challenge, emphasizing that a more serious focus on administration, adequate training for non-clinical staff, and strategic investment in IT systems are essential for improving patient experiences. Establishing measurable targets, such as patient satisfaction with NHS services, can further drive accountability and prioritize non-clinical elements in comprehensive healthcare reform.
What's the Solution?
According to the report, there are three key solutions proposed to address the communication challenges:
- Expansion of care coordinators and improved access to clinicians for complex conditions.
- Implementation of care navigators in GP surgeries to assist patients in navigating complex systems.
- Enhancement of the NHS App's functionality and publicity to increase uptake.
How can EBO help?
EBO bridges the communication gap in healthcare and places conversation at the heart of its solution. We help healthcare providers to automate patient facing processes end-to-end, thus releasing efficiency, increasing work capacity, reducing costs, and enhancing patient communication. Here's how:
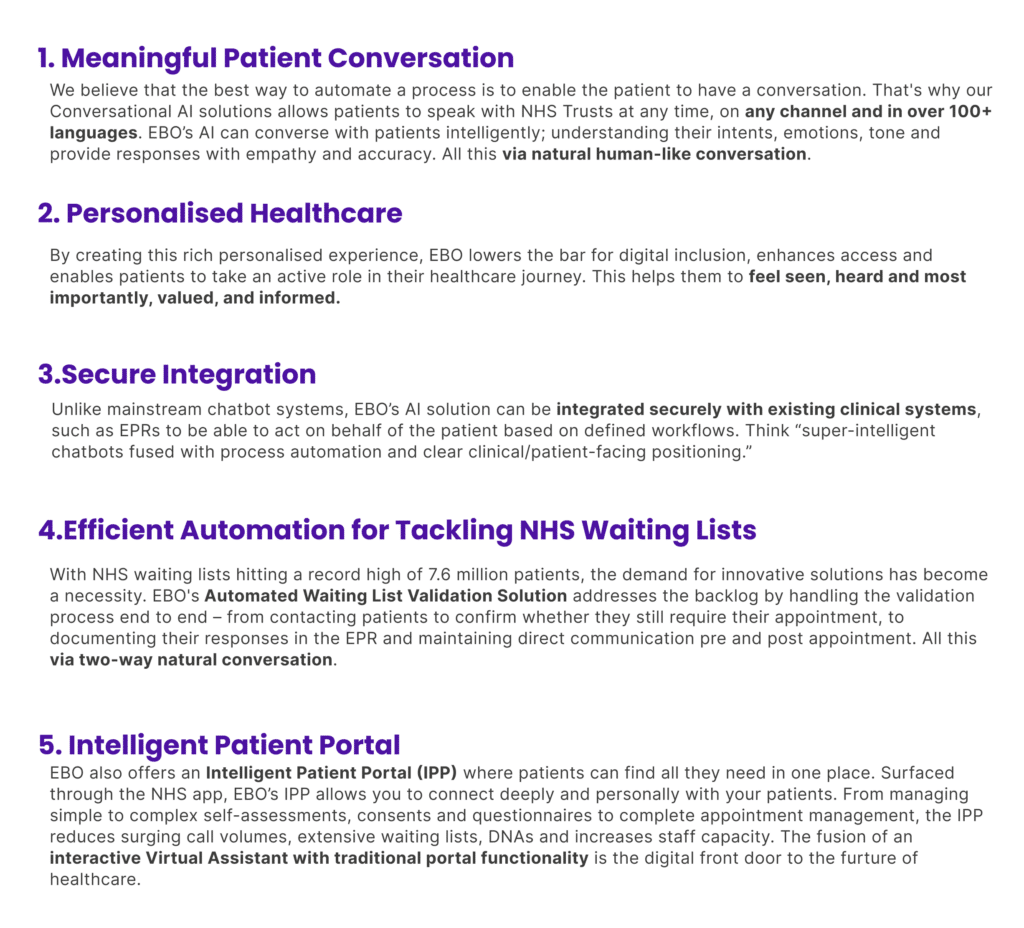
Let EBO be your partner in creating a healthcare future where effective communication leads the way in positive transformation. Discover the capabilities of EBO's AI-powered solutions, designed to enhance your patient engagement. Take action now and be part of the solution! Contact us today or download our AI guide to find out more.


